FST JOURNAL
Edge Technologies
DOI: https://www.doi.org/10.53289/HLCP6906
How AI can support those living with dementia
Professor Payam Barnaghi

Professor Payam Barnaghi is Chair in Machine Intelligence Applied to Medicine and Deputy Head of Division of Neurology in the Department of Brain Sciences at Imperial College London. He is Great Ormond Street Hospital and Royal Academy of Engineering Research Chair in Machine Intelligence for Medicine and a Principal Investigator and Group Lead for Translational Machine Intelligence in the Care Research and Technology Centre at the UK Dementia Research Institute. His main research goal is to develop AI and machine learning solutions for healthcare and create affordable and scalable digital systems that can be applied across a range of health conditions.
Summary:
- There are close to a million people affected by dementia in the UK. One in four hospital beds are occupied by somebody living with dementia and around 23% of these hospital admissions are due to preventable causes
- A lot of our work focuses on using edge and Cloud technologies to develop new care and support solutions for people living with dementia
- We train machines to look at patterns and learn how these patterns associate with different conditions
- It is important to evaluate technology and data as if you do not, your algorithm can start biasing towards a subgroup in your study.
I am a computer scientist and over the past seven years, most of my work has focused on using off the shelf technologies to monitor and support people living with dementia in the UK.
There are close to a million people affected by dementia in the UK. One in four hospital beds are occupied by somebody living with dementia and around 23% of these hospital admissions are due to preventable causes. Some of the main causes of hospital admissions are falls, hip fractures, respiratory problems and urinary tract infections (source: Alzheimer’s Society). UTI can be treated with antibiotics, but when you factor in the complex nature of the neurodegenerative, degenerative process of dementia as a disease, there is often a lot of difficulty communicating symptoms, and this makes dementia care difficult and challenging. People living with dementia are more prone to go to hospital and if they go to hospital are more prone to have adverse outcomes like having a fall. Anecdotally, you may hear that when people living with dementia go into hospital, usually they decline when they come out.
Edge Technologies for dementia
A lot of our work focuses on using edge and Cloud technologies to develop new care technologies for people living with dementia. Some of the technology we use are sensors to create something which we can continuously monitors people's sleep, physiology and movement around the house. This helps us to build a picture of their day-to-day activities and then look for anomalies, or try to look at for patterns if a person has a specific condition. With generous funding from the Department of Health and NHS, my colleagues, Ramin Nilfrooshan, Helen Rostill and their colleagues in the Surrey and Borders NHS Trust and I worked on the first generation of our in-home monitoring technologies for dementia.
In principle, these sensors are passive infrared sensors, like back door burglar alarms; when you walk in front of it, it starts sending an alert to a Cloud environment. There are also sensors for when someone is sleeping in a bed, which monitor heart rate and breathing rate, and this information is continuously collected and transferred via a secure network to the Cloud-based platform. Within the platform, we (there is some human involvement) run some analytical algorithms which do the analysis, and create alerts. We have a monitoring team who look at this information and are able to apply it to their clinical protocols and at the same time, record everything.
As soon as you start collecting data and labelling incidents, we can reverse engineer this and create more enhanced algorithms. The study, which has been running for the past 4 years, has now moved to an initiative supported by the UK Dementia Research Institute called Minder, which is led by my colleague Professor David Sharp.
Screening vs diagnostics
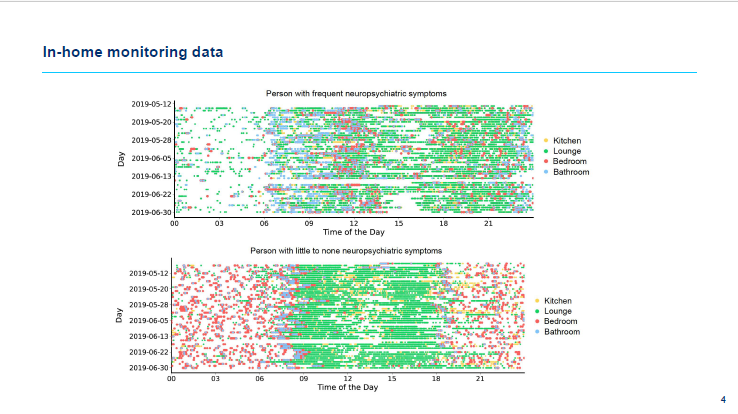
Just to take a sub set of this data: in this graph, the x axis is time of the day and the y axis are different days. These are two real patients anonymous data. Each colour shows movement in one area of the house. Here, one of the participants has a lot of activity at night and relatively stable patterns during the day. The other also has nighttime patterns but most of these are bathroom visits and in the daytime, there are lots of inconsistencies in the data.
The second participant is someone with a urinary tract infection and one of the symptoms of urinary tract infections is that people get up and go to the bathroom more often. In any case, just by looking at data you can see nighttime disturbances and someone who wanders around the house at night is at high risk of falls. I’ve picked two obvious examples here but not all of the data is so clear and it is not scalable. The work we have been doing over the past few years is to train machines to look at these patterns and learn how these patterns associate with different conditions very quickly.

Some of the symptoms of a Urinary Tract Infection are going to the bathroom, temperature and heart rate increase, and changes in breathing rate at nighttime. These are things we can pick up with our sensors. However, technology here is the easy part. Getting the right data and the right clinical insight is the most important thing. We have created an algorithm that looks at how accurate a model is by generating an alert to flag the risk of somebody having a urinary tract infection. This is not a clinical diagnostic tool, but it can be used as a screening tool, and our clinical team can take a urine sample and send it to a lab. At the same time, in parallel, a group of my colleagues are working on creating a home test.
In a post-analysis, we were interested in accuracy and demographics. We found that those who slipped through the net were generally female women aged over 65. This demographic is at higher risk than men of having a urinary tract infection. It is important to evaluate as if you do not, your algorithm can start biasing towards a subgroup in your study. We must be careful not to create a set of technologies that can discriminate.
